ACHIEVING TRANSFORMATIVE RESULTS IN FRAGILE SETTINGS
BACKGROUND
IMA implements highly effective, contextually appropriate projects to improve maternal and child health in the Democratic Republic of Congo, Haiti, Kenya, South Sudan and Tanzania.
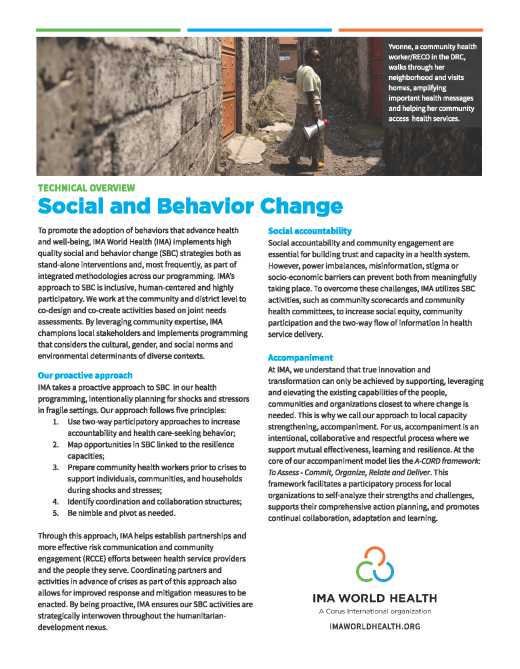
In DRC, IMA’s strong local partnerships and decades of experience enables us to provide integrated primary health care interventions across 52 health zones and consistently surpass targets for maternal and child health—despite recurrent conflict and insecurity. In South Sudan, IMA ensured access to high impact primary health care services for approximately 3.1 million people in the two most geographically challenging regions, while systematically strengthening the capacity and function of the Ministry of Health and 29 county health departments. In Kenya, IMA works closely with the Nairobi County and Sub-County Health Management Teams to provide training, continuous medical education and support to work improvement teams at 53 urban maternity wards to scale-up and improve emergency obstetric and newborn care, focused antenatal care, post-natal care and essential newborn care. IMA also works with the government to manage extensive supply chains within Haiti and Tanzania through the USAID ENVISION mass drug administration program, ensuring millions of de-worming and Vitamin A doses are distributed effectively and tracked each year.
IMA also works to increase access to quality facility- and community-based integrated management of childhood illness, immunization and diarrheal-disease management services. IMA’s nutrition programs are implemented through existing local systems for maximum sustainability, including government systems, faith-based networks, local community groups, and community-level structures. Through the Addressing Stunting in Tanzania Early (ASTUTE) program, IMA works with district multi-sectoral nutrition steering committees to strengthen their ability to coordinate, resource, and monitor nutrition outcomes, resulting in greater ownership, sustainability and service quality.
Highlights from our programs
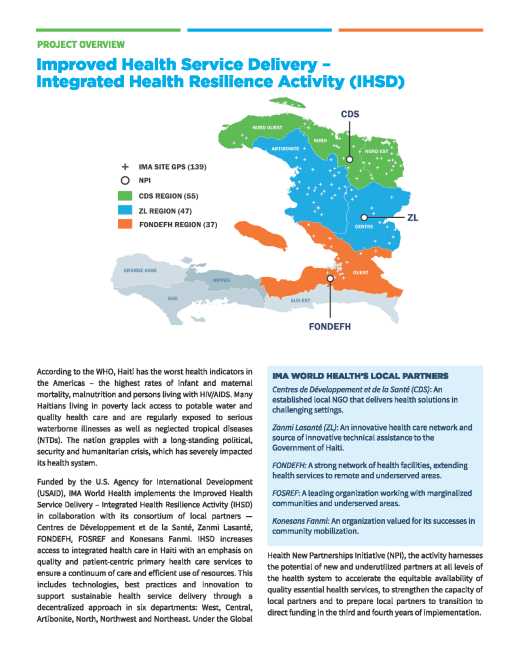
MOMENTUM Integrated Health Resilience (2020-2025): IMA World Health leads the five-year, USAID-funded MOMENTUM Integrated Health Resilience project, which is part of a suite of innovative MOMENTUM awards designed to holistically strengthen quality voluntary family planning (FP), reproductive health (RH), and maternal, newborn, and child health (MNCH) in host countries around the world. Working alongside local organizations, governments, and humanitarian and development partners in fragile settings, the project helps accelerate reductions in maternal, newborn, and child illness and death by increasing the capacity of host country institutions and local organizations—including new and underutilized partners—to introduce, deliver, scale up, and sustain the use of evidence-based, quality MNCH/FP/RH care. Learn more.
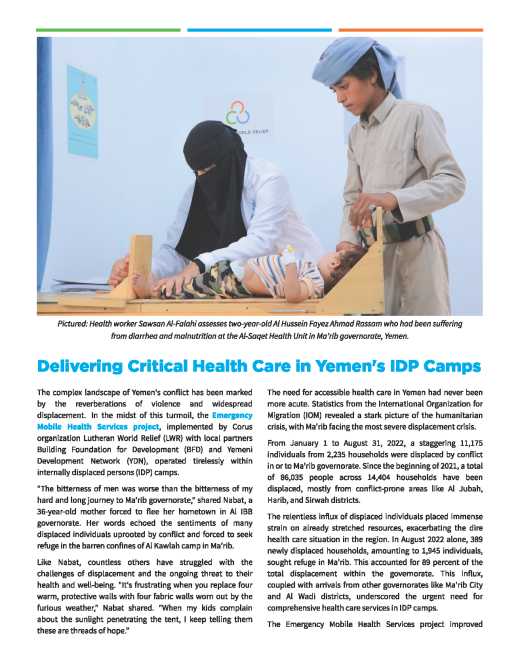
Access to Primary Health Care Project (ASSP) (2012-present): In the DRC, WHO estimated maternal mortality in 2013 at 730 per 100,000 live births and infant mortality at 97 per 1,000 live births. Through ASSP, which supports health care for a population of 8 million people in 52 health zones, IMA prioritizes delivering essential health packages that improve maternal, newborn and child health. Using an integrated and comprehensive approach, the project helps train health care workers in antenatal care and safe delivery, including delivery of emergency obstetric and neonatal care services. Our health systems strengthening approach builds local capacity and ownership of health service delivery, creating stability in an often unstable environment. For example, despite health center closures and other service disruptions in the 2017 fiscal year due to conflict and population displacement in project areas, IMA and partners achieved 102 percent of ASSP’s annual target for the number of births attended by skilled personnel at a health facility—continuing a trend of increase across five successive quarters. Additional key achievements include:
- Facilitated close to 1.5 million deliveries with a skilled birth attendant, increasing coverage from 62 percent to 80 percent
- Remarkably, in year 5, 100 percent of expected births were managed by a skilled attendant
- Financed over 200 nurses to get a university-level degree in midwifery, an area of expertise lacking in the health workforce in DRC
- Vaccinated over 1.4 million children against measles and achieved 96 percent coverage of children under one year of age, which exceeds the initial program target of 90 percent
- Distributed more than 2.26 million long-lasting insecticide treated bed nets (LLINs), including 754,195 through routine distribution to pregnant women and children under one year old
- Achieved 71 percent coverage of pregnant women who received two doses of intermittent preventative treatment as prophylaxis for malaria
- Recruited 1.32 million new acceptors of modern methods of family planning; achieved 110 percent of ASSP’s Year 5 target for new acceptors and 145 percent of the Year 5 target for couple years of protection, as a result of the improved availability of contraceptives and the scale-up of services
- Over 1.35 million pregnant women and children under 5 received direct and intensive nutrition intervention, likely reducing high risks of anemia during pregnancy and malnutrition-related sickness in early childhood
- 274,697 malnourished children have received five home visits (85 percent of those referred) and, among them, the overall recovery rate has risen steadily from a low of 44.5 percent in four years to the current recovery rate of 78 percent
- Procured an average of US $10 million worth of medicines per year for distribution and use at health facilities within ASSP’s 52 health zones
- Completed the construction or renovation of 253 health centers, including 79 new construction and 174 completed renovations, making it one of the largest (if not the largest) infrastructure development projects in DRC in many years. Learn more.
Provision of Reproductive Health Services Project (2014-present): In South Sudan, this UNFPA-funded project uses mobile clinics and outreach as well as strengthens local capacity to implement the Minimum Initial Service Package for reproductive health, including interventions to address gender-based violence, sexually transmitted infections and HIV services. It also supports sexual and reproductive health outreach activities in partnership with community-based organizations or support groups. Internally displaced people, who would otherwise have no access to reproductive health services, are seeking services at an average of 200 patients per month at the temporary clinic in Mingkaman, where thousands of IDPs from Jonglei are still encamped. The program includes the procurement and distribution of supplies in extremely remote areas.
Rapid Results for Health Project (2013-2018): With funding from the World Bank, IMA provided primary health care services for approximately 3.1 million people in the two most geographically challenging states of South Sudan, in large part to ensure that health care worker training and critical commodities to reduce maternal mortality reached some of the most rural health facilities. More than 53,000 women received at least one antenatal care visit last year and more than 27,000 children were vaccinated, despite ongoing conflict that made access and treatment difficult. In the former Upper Nile State, more than double the number of pregnant women accessed critical antenatal care. Learn more.
Afya Jijini (2015-2020): Afya Jijini, which translates to “health in the city,” is a three-year USAID contract (with two option years) with the strategic goal of improving Nairobi City County’s institutional and management capacity to deliver health services. The program improves access to and use of maternal, neonatal and child health services; family planning and reproductive health services; water, sanitation and hygiene; and nutrition services. The program has also helped the government roll out newly-revised IMCI guidelines and improve the coverage and reporting on childhood immunization in Nairobi County. In its first year alone, the USAID-funded Afya Jijini project supported Nairobi City County to scale up and make maternal and child health services available not just five but seven days a week at 35 of the county’s busiest sites. More than 3,000 mothers were reached with focused antenatal care and other maternal, neonatal and child health services as a result of the availability of weekend services. An additional 7,000 children benefited from weekend child health interventions. Learn more.
EmOC South Sudan (2010): With funding from the USAID Office of Foreign Disaster Assistance, IMA designed the Emergency Obstetric Care Program to reverse the trend of maternal mortality in vulnerable areas of South Sudan by increasing the number of facilities in the former Upper Nile State that provided EmOC services and to reverse the trend of home births by providing competent and viable birthing alternatives for isolated communities. In collaboration with the State Ministry of Health, through this project IMA established EmOC services for returnees and the local population in five targeted counties—where there was previously no coverage—through the rehabilitation of health facilities, training of health personnel, ensuring the availability of necessary medical supplies and improving information systems through case management and monitoring practices. Learn more.