Around the world, nutrition plays a significant role in children's health and well-being. Nearly half of all deaths of children under five are attributable to undernutrition, totaling more than 3 million children per year. Inadequate nutrition during a child's first 1,000 days from conception to age two can also result in chronic undernutrition (also known as stunting), which is associated with lower labor productivity, impaired cognitive ability and academic achievement.
Globally, IMA World Health addresses malnutrition through social and behavior change (SBC) interventions while strengthening policies and health systems. We support national programs, working with local authorities and community organizations to implement evidence-based approaches that transform health outcomes.
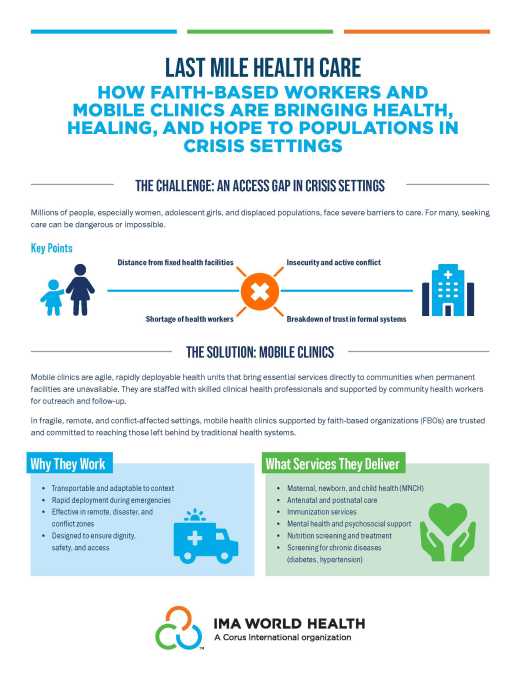
IMA World Health works to create sustainable change in the services and systems that impact nutrition through:
- Health systems strengthening that enables governments and civil society organizations (CSOs) to deliver quality nutrition services, even in hard-to-reach areas. We strengthen local capacity to address the numerous causes of child stunting and support quality nutrition services at scale.
- Multisector integration that approaches nutrition holistically and addresses the multiple causes of malnutrition, including poor food, care and health. We do so by reducing HIV/AIDS, addressing violence against women and girls, reinforcing early childhood development, and strengthening water, sanitation, and hygiene (WASH) systems and household practices. By linking nutrition with government programs and leveraging the expertise of our Corus International partners Lutheran World Relief, CGA Technologies and Ground Up Investing, we advance long-term impact on dietary diversity and food security.
- Technical assistance that supports donors and governments to develop and implement nutrition policies and programs in fragile settings through advocacy, health systems strengthening and operations research. We strengthen the evidence base around nutrition interventions and improve program design and implementation.
Project Highlights
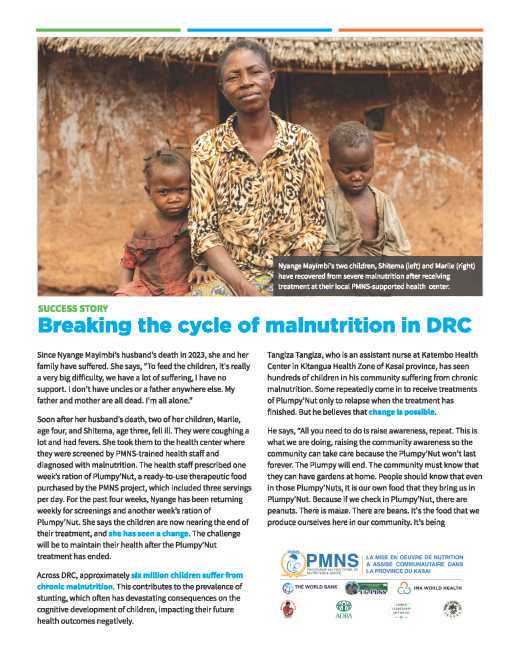
The Multisectoral Nutrition Project (Projet Multisectoriel de Nutrition et de Santé - PMNS) is strengthening nutrition outcomes for at-risk pregnant women and malnourished children in Kasai Province, DRC. With funding from the World Bank and the DRC's Ministry of Public Health, Corus organization IMA World Health and its consortium of partners are providing nutrition services at the community level, strengthening prenatal consultations as well as revitalized preschool consultations including improved routine micronutrient supplementation, and supervising systemic intensive screening and structured home visits by community health relays. The DRC's Ministry of Health and National Nutrition Program (PRONANUT) are included in all training, monitoring and evaluation, and supervision activities to encourage synergy. Within the project, IMA World Health employs its experience supporting village savings and loan associations (VSLAs), improved cook stoves, and entrepreneurship and leadership opportunities that promote home gardening and income-generating activities for women. IMA World Health's consortium of partners for the PMNS project includes the Adventist Development and Relief Agency (ADRA), SANRU, Programme for the Development of Eastern Kasai (PRODEK), and the Congo Leadership Initiative (CLI).
To date, the project has reached 408,068 children aged 0-59 months with preschool consultations and screened 26,473 children for acute malnutrition. In the first quarter of the project (August–Sept 2023), 257,125 children aged 0-23 months received a preschool consultation, 26,473 children 6-59 months were actively screened for acute malnutrition, 787,624 home visits were made by community relays to follow up with families of children screened for/diagnosed with malnutrition, and 2,986 cooking demonstration sessions were held in communities.
IMA World Health leads the five-year, US government-funded MOMENTUM Integrated Health Resilience project, which is part of a suite of innovative MOMENTUM awards designed to holistically strengthen quality maternal, newborn, and child health in host countries around the world. This includes refining the Emergency Nutrition Network (ENN)'s strategic direction, coordinating with governments and other implementers through the MAMI Global Network and MAMI Implementers' group, and providing global technical leadership around growth monitoring and promotion among children under two years of age.
MOMENTUM Integrated Health Resilience’s Enhanced Growth Monitoring and Promotion (GMP) research, policy advocacy and technical assistance equips health workers and caregivers to identify early-stage growth faltering and provide supportive interventions before malnutrition has advanced. GMP will be assessed in two West African countries and use research findings to co-develop new GMP tools, trainings for community and facility health workers and referral systems. Expert consultation on GMP that includes policymakers, implementers and academics will integrate best practices and validate and share learning from West Africa to address GMP challenges globally.
Through a DFID (now FCDO)-funded contract (2015-2021), IMA partnered with the Government of Tanzania and 50 CSOs to scale nutrition support to approximately 15% of Tanzania’s population (8.43 million people) and reduce stunting of children under five by 7% or more in four Lake Zone regions. In support of Tanzania’s commitment to the Scaling Up Nutrition (SUN) movement, IMA strengthened the capacity of local government authorities across sectors to address the myriad causes of child stunting and contributed to the evidence base for what works best and most cost-efficiently in the local context.
Through ASTUTE, nearly 7,800 district health workers and non-health sector service providers were trained and three million mothers, caregivers and decision-makers were reached with improved child feeding information. The ASTUTE project created lasting change in Tanzania, including a Stunting Reduction Toolkit that continues to support Tanzania’s National Multi-sectoral Nutrition Action Plan II (NMNAP II) implementation with English and Swahili tools like Personalized Support Group guides, radio spots, and health worker home visit guides. ASTUTE used qualitative and quantitative research to refine and scale-up SBC approaches such as PDH and engagement of male caregivers in tasks such as child feeding, developmental play, and helping with household chores. Male involvement was addressed across ASTUTE, most impactfully through SBC tactics such as community dialogues and faith leader engagement. IMA partnered with 50 CSOs and 41 LGAs to deliver nutrition services and reach over 17.6 million people through local radio (the dominant rural mass media). ASTUTE results include a 24.1% increase in the prevalence of exclusive breastfeeding with a 45% increase for children aged 4-6 months (for whom breastfeeding normally declines rapidly). Maternal nutrition and care improved dramatically including mothers being 3.3 times more likely to consume a varied diet and 1.5 times more likely to receive help from their partners.
Through the US government-funded Afya Jijini project (2015-2021), IMA strengthened Kenya's National Nutrition Center (NCC) systems to reach over 2 million women and children with high-impact nutrition interventions. Service coverage (proxy indicator Vitamin A supplementation) increased from 53% to 94% and routine monitoring of people living with HIV’s nutritional status increased from 65% to 95%. Afya Jijini provided mentorship on nutrition technical guidelines and needs-based training and coaching at 189 integrated management of acute malnutrition (IMAM) sites and 29 HIV comprehensive care centers (CCCs). Supportive supervision helped sites address long-standing challenges such as nutrition information management and helped sub-county health management teams integrate nutrition services into various health facility departments to save time for both provider and client. At the leadership level, Afya Jijini strengthened key elements of the county and sub-county health system, including dramatically improved nutrition coordination. Functional Nutrition Coordination Forums are in place as a result, guided by County Nutrition Action Plans to support multi-sectoral collaboration. Afya Jijini’s innovations include CHV-led “community conversations” to help communities tackle harmful traditional practices.
In the Democratic Republic of Congo (DRC), IMA’s FCDO (formerly DFID)-funded Access to Primary Healthcare (ASSP) project (2012-2019) and its follow-on Support to the Health System in the DRC (ASSR) project (2019-2021) reached over 7.5 million children and pregnant women including over 1.4 million nutrition intervention participants. IMA and our partners trained over 10,700 community health workers and nurses in malnutrition screening, nutrition education, and/or home gardening. Service utilization rates across 1,500 health facilities increased from 34% to 62% in six years through innovations such as reinforcement of community management of acute malnutrition (CMAM) with community relays (RECOs) and Infant and Young Child Feeding (ANJE) support groups which increased screening numbers and family support. Multi-sector malnutrition management initiatives promoted easily grown, nutrient-dense perennials such as moringa and chaya and complex carbohydrates like cassava through nurseries and demonstration gardens at health clinics.
With funding from the USAID's Bureau of Humanitarian Assistance (formerly OFDA), IMA conducted nutritional activities (2018-2020) in seven facilities in five conflict-affected counties of South Sudan in response to the growing need for an integrated response to acute malnutrition. Health services for 200,000 IDPs were provided and over 31,000 children were screened through CMAM initiatives. Activities included community outreach and screening for early detection and treatment of acute malnutrition; inpatient and outpatient management for children with severe acute malnutrition (SAM); and supplementary feeding programs for children with moderate acute malnutrition (MAM), discharged SAM patients and at-risk pregnant and lactating women.
IMA implemented the National Nutrition Communications Campaign (NNCC), a four-year (2014-2018) communications and behavior change project focused on reducing stunting, as part of Indonesia’s national strategy within the SUN movement. NNCC was a component of the larger Community-Based Health and Nutrition to Reduce Stunting Project, funded by the Millennium Challenge Corporation. NNCC worked in collaboration with the Government of Indonesia in 11 districts to increase awareness and understanding of the causes, symptoms, long-term implications and prevention of childhood stunting among parents, community members, Ministry of Health personnel, government officials and the general public; gain commitment from a broad array of stakeholders to tackle the problem of stunting; and foster individual and community behavior change related to health and nutrition among parents, caregivers and government staff. Through its strategic television campaign, from November 2015 to June 2017 the NNCC reached more than 44 million viewers with its TV spots on sanitation and infant and young child feeding—far exceeding its goal of reaching 5 million viewers. In March 2018, IMA hosted 34 governors representing every province in Indonesia, 10 ministers and the Vice President of Indonesia at the nation’s first Stunting Summit, where the Government of Indonesia committed to prioritizing 106 districts to actively fight stunting. Learn more.