A Reflection on the Ground for World AIDS Day
 Shared by IMA’s Dr. January Zilabumba, IMA staff member and physician with the Local Partners Excel in Comprehensive HIV and AIDS Service Delivery (LEAD) Project
Shared by IMA’s Dr. January Zilabumba, IMA staff member and physician with the Local Partners Excel in Comprehensive HIV and AIDS Service Delivery (LEAD) Project
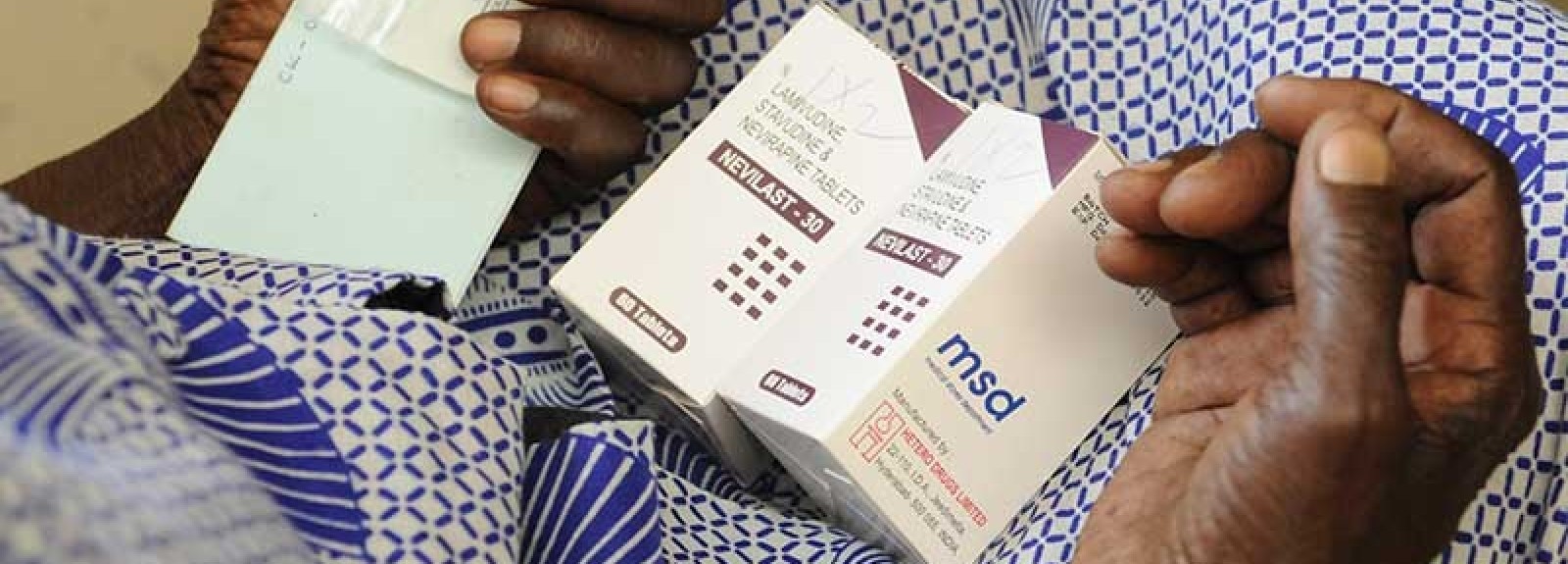
World AIDS Day offers a time to reflect on the strides we have made in the battle against the HIV epidemic. It also reminds us of the challenges we still face in realizing the “Three Zeros” (Zero New Infections, Zero AIDS-Related Deaths, and Zero Discrimination). Free ARVs, scaled up services, and committed medical staff have improved access to antiretroviral treatment (ART) tremendously in Tanzania and more broadly in Africa.
The AIDS pandemic is now 33 years gone since the first person was diagnosed with HIV. Early on, Tanzania saw a small army of people whose muscles were wasted, who experienced stigma and isolation. This was compounded by the hopelessness us healthcare professionals felt, as we could do nothing.
I still vividly recall my encounters with HIV positive clients as I began working with IMA on project LEAD four years ago. One woman who cried in front of me as she narrated her problem: She had the will to live longer, but didn’t have the money to access her HIV treatment:
“Doctor, I am living in absolute poverty,” she said. “I have to take medication every month at either Shirati hospital, which cost me Tsh 15,000 (about $7), or have to go to Musoma. It’s relatively cheaper, but I have to board the boat in the morning when the waves in the lake are calm, sleep in Musoma and return the following day…it is becoming unbearable to me.”
Thanks to the LEAD project, we were able to allocate funds for an outreach program to a nearby dispensary that she could reach by walking and renovated the building to cater for HIV services for her and many other clients.
Our Success to Date and the Challenges We Still Face
It is so exhilarating to write that we have reached 100% coverage of Option B+ at our PMTCT sites, which means all pregnant women start ART immediately and for life upon receiving an HIV-positive diagnosis, improving the health of both mother and baby. As a result, nearly all children born to HIV-positive mothers under this project can look forward to an HIV-free life. This is thanks to continued advocacy at the clinic and within the community that ensures that pregnant women make trips to the antenatal clinic and are tested for HIV – eventually almost all mothers who test HIV-positive are initiated on ART.
We also now have several point of care equipment at our project sites like PIMA CD4 testing machines that facilitate real-time access to CD4 counts. In addition, PCR machines at the zonal referral hospital has made it possible to test babies exposed to HIV at four weeks old and start them with ART as needed and as early as possible. . All project supported health care workers are trained on ART management and all entry points within hospitals are now equipped and trained to test for HIV. Improvements in computerizing the supply chain and patient records has made it easier to handle huge amounts of data and make decisions that result in improvements to care and treatment services.
Is it the time to celebrate? We should wait a bit; we still have work to do. In Tanzania, almost 50% of pregnant mothers deliver at home, with a traditional birth attendant, where she doesn’t have access to PMTCT services. violence against women and girls is on the rise (standing around 70% in some places), as is migratory work (such as fishermen who usually travel to the lake during certain periods of the year, without access to treatment). Each of these challenges enrollment and retention in HIV services.
We still have not reached 100 percent in ensuring that every hospital, health center and dispensary has the capacity to provide HIV services. In addition, we still do not have all eligible patients on treatment, and the majority of Tanzanians do not know their HIV status. And as we move to the eligibility criteria of below 500 CD4 count for enrollment on HIV treatment, we are still even struggling to capture all who are below 250 CD4 count. Attrition is still a challenge as we find difficulty in retaining our clients in treatment. Despite improvements, there are still large numbers of those who are lost to follow-up or fail to achieve treatment success. We must think out of the box, working with other medical and social service departments to stop attrition, like linking hospitals with the community in a manner that ensures referrals.
We also witness shortages of important TB diagnostic tools, like the GeneXpert machine. This machine has higher sensitivity and specificity than traditional microscopy, reducing the likelihood for TB infections to be undetected.
And our program, like so many other programs, has made little progress to attract adolescents who are HIV-positive. Now we have started special clinics for them that feature confidential, attractive and engaging services. We plan to scale this up in 2016 to help identify teenagers living with HIV.
A Promising Road Ahead
Yet despite these challenges, it is so exhilarating to write that we have reversed the alarming rise in new infections and overall HIV prevalence in Tanzania, dropping from seven to 5.3 percent during the past 10 years. We are close to the tipping point where we shall have a positive balance in which clients started on ARVs are outnumber those with new infections, creating a path toward an HIV-free future. As we turn the page into 2016, I look forward to continuing this fight and to achieve the Three Zeros.